The copyright of this article belongs to Siansonic Technology.The production is prohibited without permission.
HIFU focused ultrasound provides a non-invasive, safe and effective physical therapy in clinical applications. HIFU focused ultrasound is a non-invasive, safe and effective physical treatment method in clinical application, which utilizes the physical properties of ultrasound such as directionality/focusability and penetrability, and focuses the ultrasound on the diseased tissues in vivo through HIFU focused ultrasound, resulting in irreversible coagulative necrosis of the target tissues due to the denaturation of the proteins. HIFU focused ultrasound, as a non-invasive, safe and promising treatment modality, has been widely used for both malignant tumors and benign diseases. The Clinical Application Guidelines for High Intensity Focused Ultrasound Tumor Therapy System (Trial) issued by the Chinese Medical Association in 2005 stipulates that HIFU focused ultrasound is suitable for the treatment of solid tumors of tissues and organs, including liver tumors, breast tumors, uterine fibroids, uterine adenomyosis, benign prostatic hyperplasia and prostate cancer.
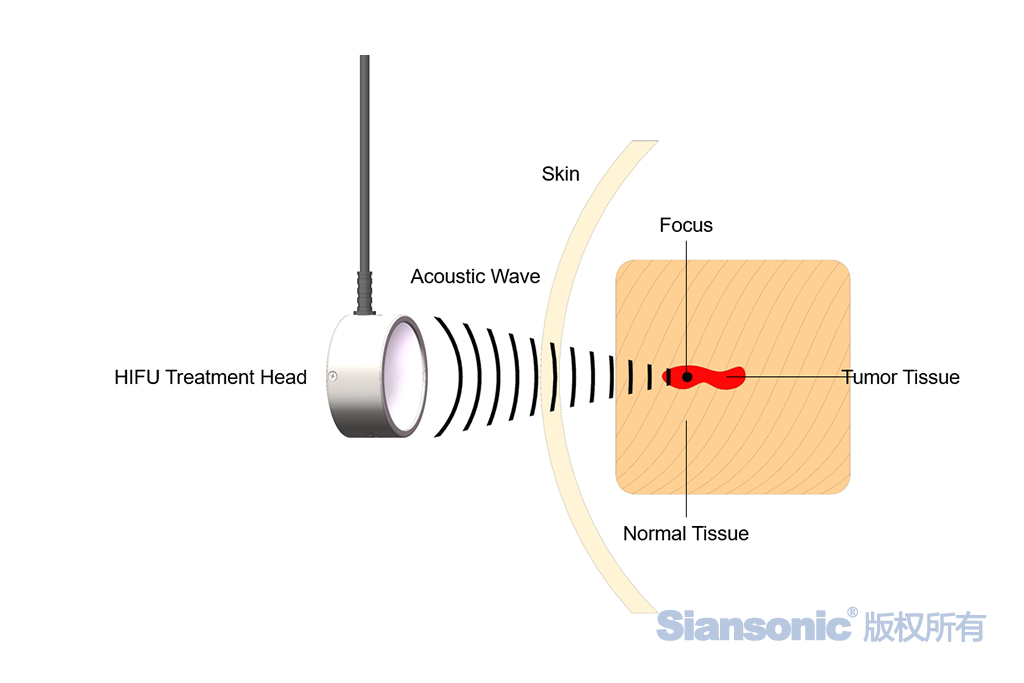
Figure 1. The principle of tumor treatment used by focused ultrasound
1. HIFU focused ultrasound has long been used for the treatment of primary and metastatic liver tumors. The high safety profile of HIFU focused ultrasound allows a small percentage of Child-Pugh C cirrhotic patients who are not candidates for transcatheter arterial chemoembolization to undergo liver transplantation. Evidence suggests that the transcatheter arterial chemoembolization technique combined with HIFU focused ultrasound has a higher overall remission rate in the treatment of primary hepatocellular carcinoma, kills tumor cells adequately, reduces the rate of local recurrence and metastasis after surgery, and has fewer adverse effects, and when compared with transcatheter arterial chemoembolization technique alone for the treatment of liver tumors, the combination of HIFU focused ultrasound Compared with transcatheter arterial chemoembolization alone in the treatment of liver tumors, combined with HIFU focused ultrasound treatment has higher long-term survival rate.
2. Breast cancer and fibroadenoma are most conventionally treated by surgical excision of the lesion. HIFU focused ultrasound is an effective non-surgical treatment for patients at high risk for surgery and those who want to preserve their breasts. It is reported that the 5-year disease-free survival rate and recurrence-free rate of 22 breast cancer patients treated with HIFU focused ultrasound were 95% and 89% respectively.
3. Prostate cancer is one of the most common causes of cancer-related deaths in men, and benign prostatic hyperplasia is one of the most common diseases in middle-aged and elderly men. Because HIFU focused ultrasound has the advantages of low anesthesia requirement/low risk of infection, HIFU focused ultrasound has been successfully applied to BPH treatment for patients who are old and frail with other comorbidities and obvious contraindications to surgery, causing irreversible changes in prostate tissue.
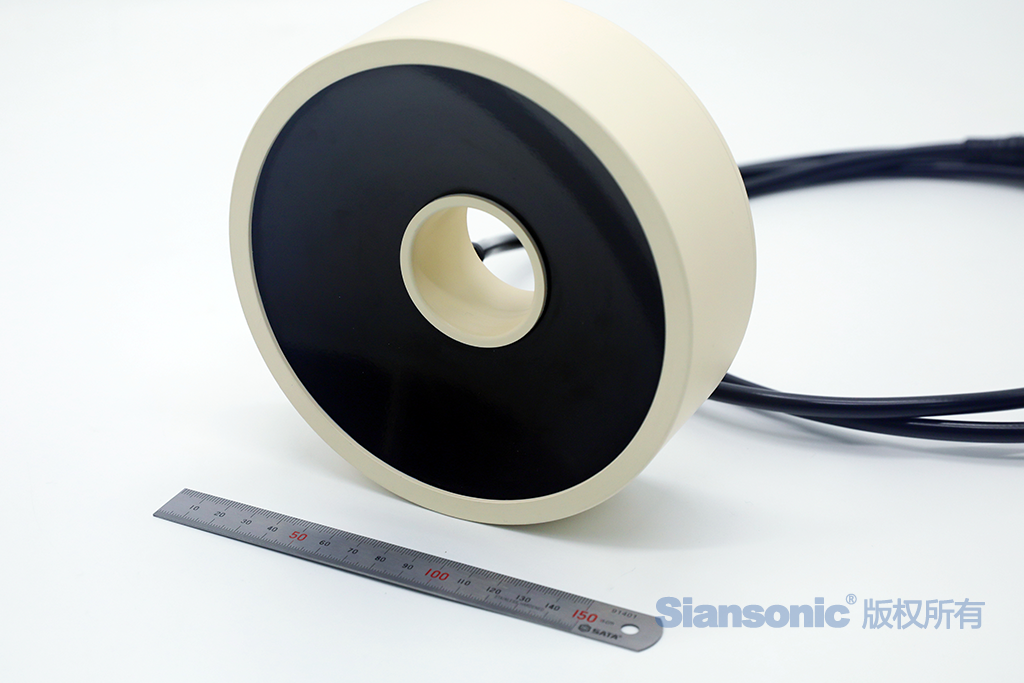
Figure 2.HIFU focused ultrasound transducer
4.Since HIFU focused ultrasound has been applied to the clinical treatment of uterine fibroids, some studies have confirmed that the fibroids and uterine volume of patients who have been treated with HIFU focused ultrasound for 2 years postoperatively have shown a trend of shrinkage, and the symptoms and the quality of life have been significantly improved after surgery compared with that before surgery. HIFU focused ultrasound, as an effective and safe treatment for symptomatic fibroids, is a good treatment option for women of reproductive age who want to preserve their uterus. And, for patients with secondary myomectomy, HIFU focused ultrasound treatment provides longer-term symptomatic relief, longer intervals between re-interventions, and a lower complication rate than secondary myomectomy. Patients who choose HIFU focused ultrasound treatment have a lower risk of anesthesia, lower risk of postoperative infection, shorter hospital stay, and faster postoperative recovery than other treatment modalities.